Unlock Your Potential Today
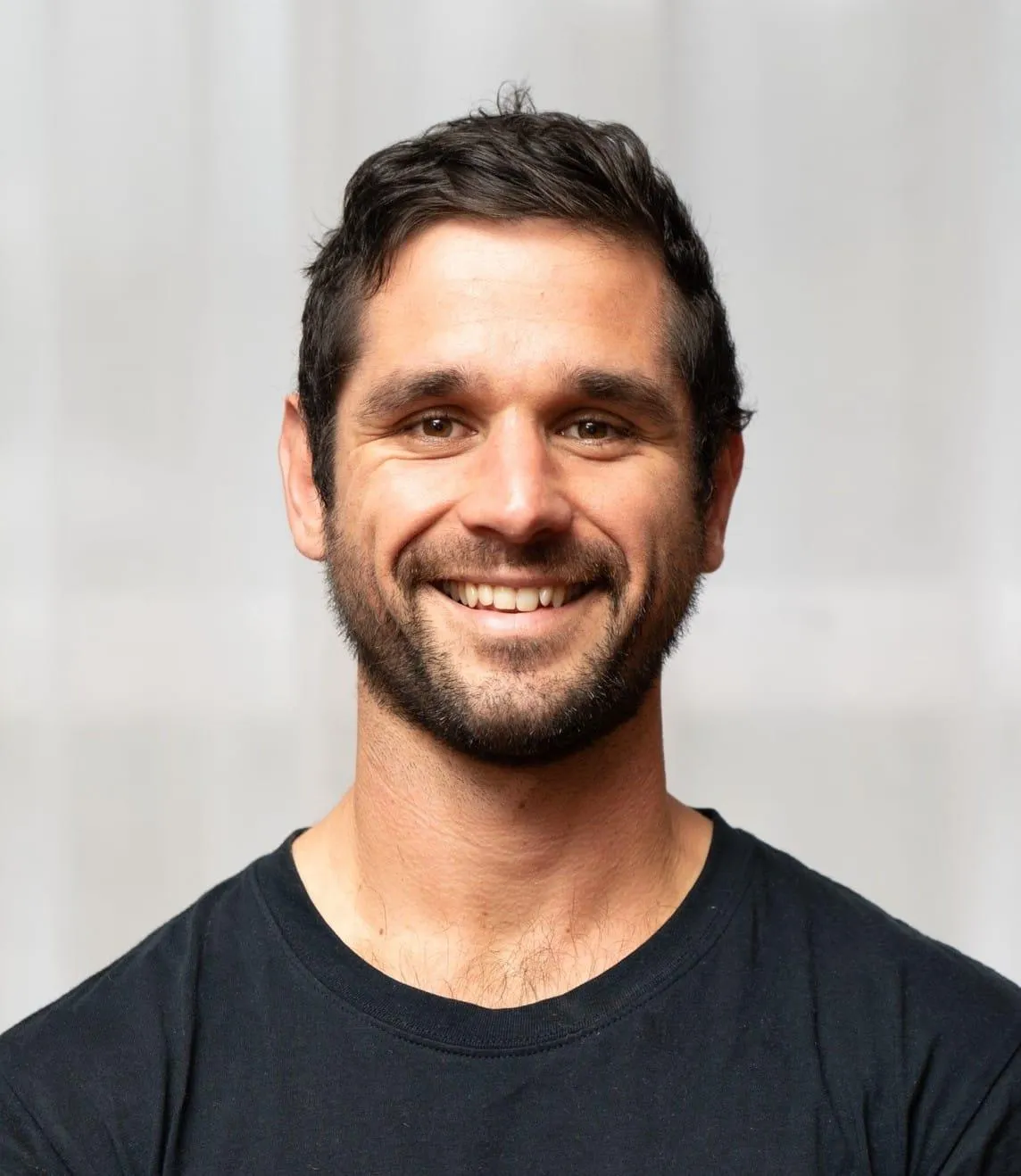
THE FOUNDER OF PRIMALTHENICS
Chris Miller is a multidisciplinary performance coach with over 20 years of experience across health, rehabilitation, elite sport, and applied neuroscience. With a clinical foundation as a registered Doctor of Traditional Chinese Medicine (TCM), Chris is known for his ability to transform pain, dysfunction, and injury into strength, resilience, and long-term performance.
He holds a Bachelor of Health Science and an Advanced Diploma of TCM, completing his postgraduate internship at Guangxi Traditional Chinese Medical University in China. For 15 years, Chris ran a successful clinical practice specialising in sports injury rehabilitation. His education also includes a Bachelor of Arts (History), a Graduate Diploma in Secondary Education, and postgraduate training in Sports Nutrition, Health Coaching, Functional Neurology, and Medical Neuroscience.
Since 1997, Chris has coached athletes from school level to international competition, working with Olympic and Commonwealth Games athletes (Beijing, London, Rio, Glasgow, Gold Coast, Birmingham) and elite teams including the QLD Reds, Brisbane Broncos, Australian Wallabies, Western Force, QLD and NT 7s, and world-ranked CrossFit athletes.
He has held senior leadership roles as Head of Athlete Performance and Head of Research & Development within Australian health and supplement companies, and currently leads science and product research for Hydra Longevity, an international anti-aging supplement brand.
Chris is the founder of PrimalThenics, a bodyweight-based training system integrating clinical rehabilitation, neuromuscular re-education, mobility, and primal movement. Delivered globally through the PrimalThenics App, the system focuses on sustainable strength, movement quality, and injury recovery. He is also the creator of LeanSuits Fitness, an EMS-based training model designed to deliver meaningful strength and body composition results in just 20 minutes. He is also one of only several Master Trainers in the World for Exxentric Flywheels, and is the only licensed educator for Exxentric in Australia.
Having personally overcome significant health challenges—including three right knee reconstructions and recovery from a sinus tumor with neurological complications—Chris brings rare lived insight into human resilience, recovery, and longevity. These experiences continue to drive his exploration of neuroscience-led performance and long-term health.
Alongside running the PrimalThenics Studio and delivering coach education and mentoring, Chris is a devoted husband and full-time stay-at-home father.

MEET OUR PRIMAL COACHES
With a background in elite competition swimming, Lauren has a passion for movement and sport.
She loved seeing what she was capable of and thrives on helping others work towards their goals too.
Throughout her swimming career, Lauren enjoyed yoga as a form of recovery and enhancement on her training. She found it assisted with her mental focus, balance and preparation for competitions.
Without meaning to, she became a more well-rounded athlete both in the gym and in the pool due to her improved body-awareness and strength.
In 2024, Lauren completed her 200hr Yoga Teacher Certification and now facilitates the Primal Yoga at PrimalThenics.
She loves the blend of quiet focus and challenging movements that Primal Yoga provides and is committed to helping people feel stronger, more mobile and confident in their ability.

Jo is a proud PrimalThenics Studio coach with a rich background as a former teacher, PT, Jump Rope for Heart program Co-ordinator
and a current paramedic in the Queensland Ambulance Service. Holding a cert 3 in Fitness and a Bachelor of Applied Science (Physical Education & Ambulance) she brings holistic health experience across education, training and frontline health care.
Having completed Nijmegen Four Day Marches and summiting Island Peak (6,189m) she champions functional movements, such as crawling, agility and bodyweight strength to help sustain healthy active lives.
Jo is looking forward to some 3-4 day pack walks this year and to helping all clients to build power, mobility and resilience through coaching classes.

Courtney is the Administrator and Coach at the PrimalThenics studio, bringing a rich background working with elite athletes. Currently studying a degree in Primary HPE alongside her Certificate III in Personal Training, Courtney takes charge of all junior programs within the studio while also playing a key role in the day-to-day operations of PrimalThenics.
Having competed for Australia at the Ice Hockey World Championships, Courtney’s background informs a comprehensive insight of athletic development, movement quality, discipline, and performance under pressure. This experience, combined with a passion for youth development, allows Courtney to create engaging, age-appropriate programs that build confidence, resilience, and strong movement foundations in young athletes.
Beyond coaching, Courtney’s leadership and organisational skills are central to the smooth running of the studio. From program planning and communication with families to supporting coaches and maintaining high standards across all junior and senior offerings, Courtney helps ensure PrimalThenics operates with professionalism, care, and a strong community focus.

Todd MacDonald is the General Manager of PrimalThenics and Head Coach of Partnerships, working to build meaningful relationships that extend the reach and integrity of the practice. He is also a PrimalThenics and LeanSuits coach, with a deep interest in functional strength, injury prevention, and long-term physical resilience.
He has worked as a CEO in the arts sector and now works as a professional corporate coach, actor, leadership mentor, and trainer. His background as an actor informs a deep understanding of presence, clarity, and how the body shapes the way we think, lead, and relate. This intersection of leadership, performance, and movement underpins his approach to both coaching and training.
At the heart of Todd’s work is the belief that we must return to the body—not as something to fix or discipline, but as a source of intelligence. He is committed to helping people make movement a daily, meaningful habit rather than a chore, supporting strong, adaptable bodies capable of meeting the demands of modern life with resilience and ease.

Nathan Tomarchio is the Head Coach at Primalthenics and an accredited Exercise Physiologist with over 10 years’ experience in the allied health and fitness industry.
At Primalthenics, Nathan works alongside founder Chris to create and deliver youth and adult programs, facilitate land-based training for the Newmarket Junior National Swim Squad, and provide one-on-one coaching for individuals looking to address root causes and improve their health and performance.
Nathan has been with the team for over three years and was drawn to Primalthenics for its unique blend of Eastern medicine, neural engagement therapy, mobility and animal flow, and innovative approaches to strength and conditioning, including the use of exxentric flywheels and K-boxes.
Nathan’s passion for health led him to study through the CHEK Institute, completing Holistic Lifestyle Coaching Level 1 and Integrative Movement Science Level 1. These frameworks, combined with the Primalthenics system and his Exercise Physiology background, form the foundation of his one-on-one work.
He works closely with clients to build strong foundational health principles, reduce physiological load, and improve functional capacity, empowering them to take ownership of their health and do more of what they love.
In addition to his role at Primalthenics, Nathan is the Head Exercise Physiologist at The Foot Collective, an international organisation leading the way in foot restoration, balance, and play-based movement training. He has also completed rotational movement training through the WECK Method, incorporating concepts such as the coiling core and rope flow into both his personal practice and professional coaching.
Drawing from these modalities — alongside a grounded, playful approach — Nathan brings a unique coaching style to the Primalthenics studio.
If you wish to work with Nathan in a one-on-one setting (health fund rebates may be available), or join him in a group class, please reach out to the Primalthenics team.
For further information email [email protected]
or call 0452 478 487
Location
Newmarket Pool,
71 Alderson St, Newmarket, Brisbane
Links
Subscribe to my newsletter
Legal notice
Cookies policy
Privacy Policy
Terms of use
© 2025 PrimalThenics
Serving Newmarket, Wilston, Ashgrove & surrounds